
Dear colleagues,
We apologize for being late with our news! The pandemic caused organizational problems. But finally we are pleased to offer you a choice of articles on neuromuscular ultrasound that were published in the last quarter of 2021.
Now what is going on in the world of science? We came across a lot of interesting studies! We found a lot to learn about carpal tunnel syndrome – yes, believe it or not – but there are still frontiers in this forever hot topic. You´ll hear about influence of skin temperature, effects of carpal tunnel release on mean grayscale level and nerve mobility. The vagus nerve is examined in patients with Parkinson´s disease and patients with stroke and atrial fibrillation. Furthermore, news about optic nerve ultrasound, polyneuropathies and small nerves is included.
We hope you will enjoy your read.
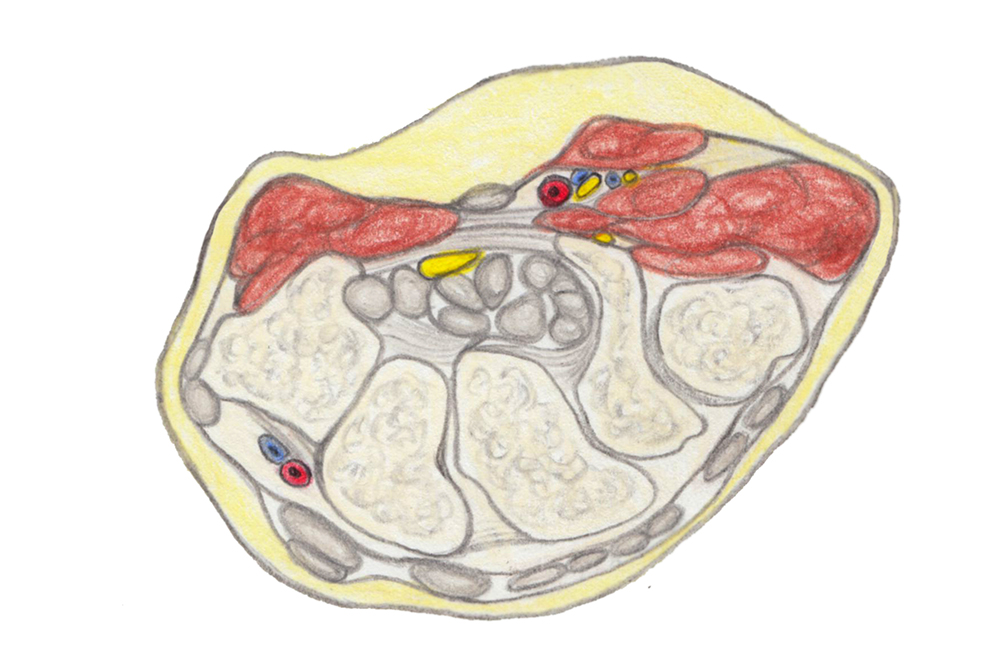
© Gerlinde Maria Gruber,2019
CARPAL TUNNEL SYNDROME & OTHER ENTRAPMENT NEUROPATHIES
Yeom et al. Cross-sectional area of the median nerve as a prognostic indicator in carpal tunnel syndrome treated with local steroid injection. J Hand Surg Am 2021 Nov 25, online ahead of print
This is a retrospective study, looking at outcomes of 40 patients with CTS after local steroid. Patients were divided into those with a CSA of the median nerve >15 mm2 (n=16) and those with a CSA <= 15 mm2 (n=24). Treatment success was defined as the absence of symptom recurrence within the entire follow up period.
This could be achieved in 45% (n=18) patients within an average follow-up of 16 months. 11 patients underwent CT release on average after 11 months of steroid injection. There was no association between success and preinjection CSA. Therefore, a large CSA does not preclude the possibility of symptomatic relief.
Hara et al. Evaluation of restricted motion area of the median nerve in patients with carpal tunnel syndrome: a new measurement method using an ultrasonographic video image. J Hand Surg Asian Pac 2021; 26(4):635-43
For this study 6 wrists of patients with CTS (before and after surgery) and 6 wrists of healthy controls were scanned in transverse view during passive wrist flexion. From the resulting videos, the authors created a motion ratio of the median nerve. The motion ratio was smaller in patients with CTS, also partially increased after surgery, but overall stayed low compared to controls. So despite improvement of symptoms, there was no change in restriction of nerve mobility, suggesting that reduced mobility is not the cause of symptoms.
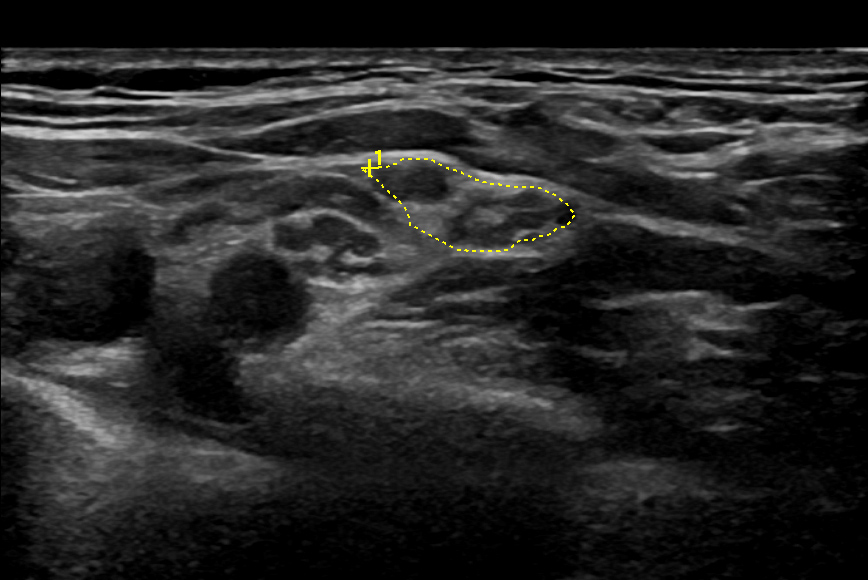
Holzapfel et al. Nerve echogenicity: changes in high-resolution nerve ultrasound in carpal tunnel syndrome after surgery. Ultrasound Med Biol 2021 Nov 10; online ahead of print
Mean echogenicity of 15 median nerves in patients with CTS was assessed before and 3 months after surgery and compared to 15 controls. Echogenicity was significantly lower in patients before surgery and increased three months after it, but did not reach the level of healthy controls.
The authors suggest that echogenicity of the median nerve may be used as a biomarker of successful carpal tunnel release.
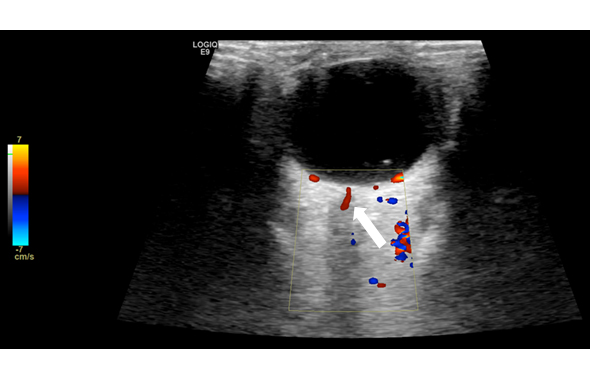
*Chang et al. Influence of temperature on sonographic images of the median nerve for the diagnosis of carpal tunnel syndrome: a case control study. BMC Med Imaging 2021; 21(1):163
This study examined whether skin temperature has a detectable effect on CSA and intraneural blood flow of the median nerve in 50 patients with CTS and 50 healthy controls. Theoretically, swelling and intraneural blood flow could be influenced by skin temperature. It turned out the CSA was stable at 30, 32 and 34°C. The power doppler signal, however, only showed a significant difference between patients and controls at 30 and 32°C, while it was lost at skin temperature of 34°C. The authors state that when residing in warm environments, power Doppler should only be cautiously interpreted in patients with warm skin temperature.
Note: Would you diagnose CTS based on detectable power doppler signal? We would be interested to hear. We consider hypervascularization something you can find, but the diagnosis is based on the swelling of the nerve – how about your lab?
Podnar S. Length of affected nerve segment in ulnar neuropathies at the elbow. Clin Neurophysiol 2021 Nov9, online ahead of print
The authors documented the length of affected ulnar nerve segments in patients with ulnar neuropathy at the elbow (UNE) by means of reduced motor nerve conduction velocity in electrodiagnostic studies and an increased cross-sectional area on ultrasound (n=194).
Both diagnostic modalities revealed an average length of around 4 cm. The affected nerve segment was longer in more severely affected patients. The author states that the length of affected nerve segment needs to be taken into account when discussing pathomechanisms of UNE.
*Wu et al. Efficacy of 5% dextrose water injection for peripheral entrapment neuropathy: a narrative review. In J Mol Sci 2021; 22 (22):12358
This review provides an overview on the currently existing papers about 5% dextrose water injection for treatment of different entrapment neuropathies. They also sum up the mechanisms which could contribute to treatment success with this method, which is currently not really known.
POLYNEUROPATHY
Bulinski et al. Neuromuscular sonography detects changes in muscle echotexture and nerve diameter in ICU patients within 24 h. J Ultrasound 2021 Dec 6, online ahead of print
The authors examined 17 ICU-patients and compared them to 7 healthy controls. They assessed gray scale values of the rectus abdominis, biceps, rectus femoris and tibialis anterior muscles together with nerve ultrasound of the peroneal, tibial and sural nerves on days 1, 3, 5, 8 and 16 after admission. Higher grayscale values were already detected at day 1 or latest day 3. The same was true concerning the nerves. The authors suggest that nerve CSA might be a useful parameter to identify patients at risk of difficult weaning. And that these findings are signs for neuromuscular suffering in the most severe patients.
Leonardi et al. High-resolution ultrasound of peripheral nerves in late-onset hereditary transthyretin amyloidosis with polyneuropathy: similarities and differences with CIDP. Neurol Sci 2021 Nov 21, online ahead of print
This small study looked at the ability of ultrasound to differentiate between hereditary transthyretin amyloidosis with polyneuropathy (ATTRv-PN) and chronic inflammatory demyelination polyneuropathy (CIDP). Overall, the CSA of the brachial plexus, median nerve, ulnar nerve and peroneal nerve were smaller in patients with ATTRv-PN than in those with CIDP. However, of the 11 patients with ATTRv-PN two had electrodiagnostic studies compatible with CIDP and they were also found to have an ultrasound result compatible with CIDP. Therefore, it was concluded that the usefulness of ultrasound as a standalone tool might be limited in theis disorder.
OPTIC NERVE
Patel et al. Ultrasound of optic nerve sheath diameter and stroke outcomes. Crit Care Explor 2021;3(11)
For this study, bilateral optic nerve sheath diameter (ONSD) was measured in 68 patients with ischemic or hemorrhagic stroke at arrival and within the first 2 days of admission. Outcomes were inpatient survival, cerebral performance category and modified Rankin Scale at 3 and 6 months. ONSD differed significantly for both stroke types between those who survived compared to those who died before discharge (0.53 vs 0.58 cm; p = 0.009 in ischemic and 0.57 vs 0.62 cm; p = 0.019 in hemorrhagic stroke patients).
Every 0.1 cm increase in ONSD increased the odds ratio for death by 4.2 in ischemic and 6.2 in hemorrhagic patients. Furthermore, increased ONSH correlated with a poor functional outcome at 3 and 6 months.
This led to the conclusion that ONSD could serve as a noninvasive marker of in-hospital mortality and functional outcome.
SMALL NERVES
*Oura et al. Cross-sectional area of the vagus nerve on carotid duplex ultrasound and atrial fibrillation in acute stroke: a retrospective analysis. eNeurologicalSci 2021 Nov 3.
The authors retrospectively reviewed axial view of carotid ultrasound at thyroid level in 150 consecutive patients with ischemic stroke or transient ischemic attack. They noted vagus nerve CSA and examined the association between vagus nerve CSA and atrial fibrillation. It turned out that the median right vagus nerve CSA was significantly smaller in patients with AF than in patients without. They suggest that patients with small right vagus nerve CSA should be closely monitored for development of AF.
*Bak et al. Comparison of ultrasound with electrodiagnosis of scapular winging: a prospective case control study. Clin Neurophysiol 2021 Oct 29; online ahead of print
21 patients with scapula alata and 41 healthy controls underwent a standardized examination including clinical examination, electrodiagnostics (EDX) and neuromuscular ultrasound of the serratus anterior, rhomboid major and trapezius muscle, as well as the long thoracic, dorsal scapular and spinal accessory nerves.
20 patients had medial winging, 6 lateral and one had both. EDX and US detected abnormalities of the serratus/long thoracic with a sensitivity of 65% and a specificity of 100% and 57%. The corresponding numbers for trapezius/SAN were a sensitivity of 60 and 40% and specificity of 91 and 86%. There was no significant difference between the methods.
In conclusion, US can contribute to diagnostic workup of scapula alata by showing muscular atrophy and nerve enlargement.
Note: The article also offers a good overview on how to examine patients clinically! We think a standardized work-up of patients with scapula alata is highly interesting. What is your opinion?
Abdelnaby et al. Vagus nerve ultrasonography in Parkinson´s disease: a systematic review and meta-analysis. Auton Neurosci 2021; 234: 102835
The vagus nerve was suggested as one of the major routes of Parkinson´s disease (PD) progression from enteric nervous system to brain. This review surveys five studies on patients with PD and CSA of the vagus nerve (patients with PD n=128, controls n=111). The CSA was smaller in PD patients with 0.29 mm2 for the right and 0.23 mm2 for the left vagus nerve. This was significant for overall effect. Therefore, the authors concluded that there is a degree of vagus nerve atrophy that could be detected sonographically with high confidence and can be used as a marker for vagus neuronal lesion or neuropathy. They suggest further studies.
*Shi et al. Sonographic features of the lateral femoral cutaneous nerve in meralgia paraesthetica. Quant Imaging Med Surg 2021; 11(10): 4269-74
86 clinically suspected meralgia patients and 40 asymptomatic controls were recruited for the study. 82 (95%) of the patients had ultrasound findings compatible with meralgia. 54 showed an abrupt caliber change, 63 an indistinct perneurium and 44 an abnormal intraneural vascularity. The average value for the CSA at the level of the anterior superior iliac spine was 4.47±2.64 mm2, and the cut-off value was 2.65 mm2.
Ok… now that was a lot to go through. We hope you liked it and can use some of the information for yourself. If you have any comments or we missed your most important paper, just leave us a comment!
Stay safe, see you soon.
Your Sonocampus Team.

Hello dear I hope you are doing well, please I am interested in facial nerve ultrasound is there any near articles or preferably videos . Thank you very much
Dear Safaa Hussein, yes, there are. I sent you an email, hope this is helpful for you. Best Doris