Still in the mood for documentation….
Dear colleagues!
Welcome to part 4b of our series on how to set up your own neuromuscular ultrasound lab!
As we admitted the last time, we have to cheat a little bit and divide step 4 into two parts to get all the information across.
In the last part of our series we talked about documentation already and covered the different mononeuropathies. The blogpost can be found here:
This time we deal with documentation of the polyneuropathies. They are a different cup of tea and when they came in the center of attention in neurological research, it soon became clear that
a) ultrasound can be helpful for diagnosing especially demyelinating polyneuropathies and
b) it won´t be as easy as just scanning the affected nerve(s).
Espcially for chronic inflammatory polyneuropathy (CIDP), many diagnostic approaches were tested. Initially,
If you have comments or ideas – we are happy to hear them!
Now let´s get started. Fasten your seatbelts and get ready for the first part of our fourth chapter:
4b. DOCUMENTATION OF POLYNEUROPATHIES
a. Chronic inflammatory demyelinating polyneuropathy (CIDP) and subtypes
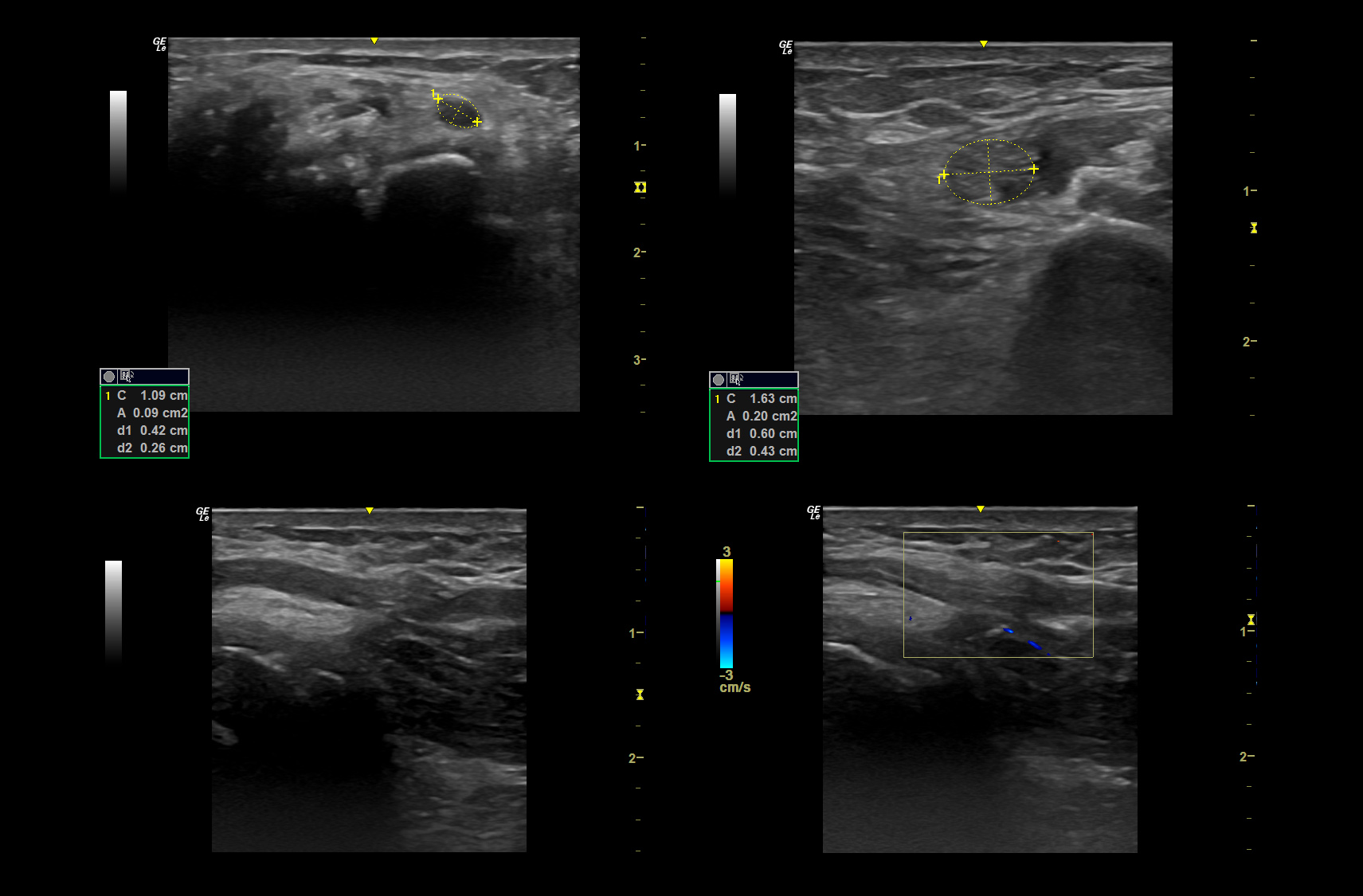
CIDP was the disease which made clear that we need to get beyond singular measurements to reach the diagnosis. Several scoring systems have been proposed in literature. The one by Goedee et al. was also included as a supportive criterion in the diagnostic guidelines of the EFNS/PNS in 2021 and may therefore be the one to stick to in daily clinical routine. It consists of measuring the cervical roots, trunks in the interscalene triangle and the median nerve on both sides (Pic 1).
The guideline can be found here:
As we came across several misunderstandings concerning the measurement of trunks, we did an extra post about this topic that can be found here: …
We suggest that if you have a symptomatic nerve to do this one as well.
If unremarkable, we usually keep pics of sites listed in the score. If you find any changes, we advise to additionally take a video across it.

Pic 1. Patient with CIDP and enlargement of
a. C5 root (CSA 25 mm2)
b. C6 root (CSA 18 mm2)
c. C7 root (CSA 23 mm2)
b. Guillain-Barre-Syndrome
If the acute form of immune mediated polyneuropathy is your differential diagnosis, the supraclavicular plexus and its roots are the most rewarding sites for scanning. Not many studies have been published on this topic, though. Patients with GBS barely ever show swelling of peripheral nerves. Catch the roots, the trunci and the supraclavicular view next to the subclavian artery in side comparison with measurements. The vagus nerve might be an indicator for autonomic failure.
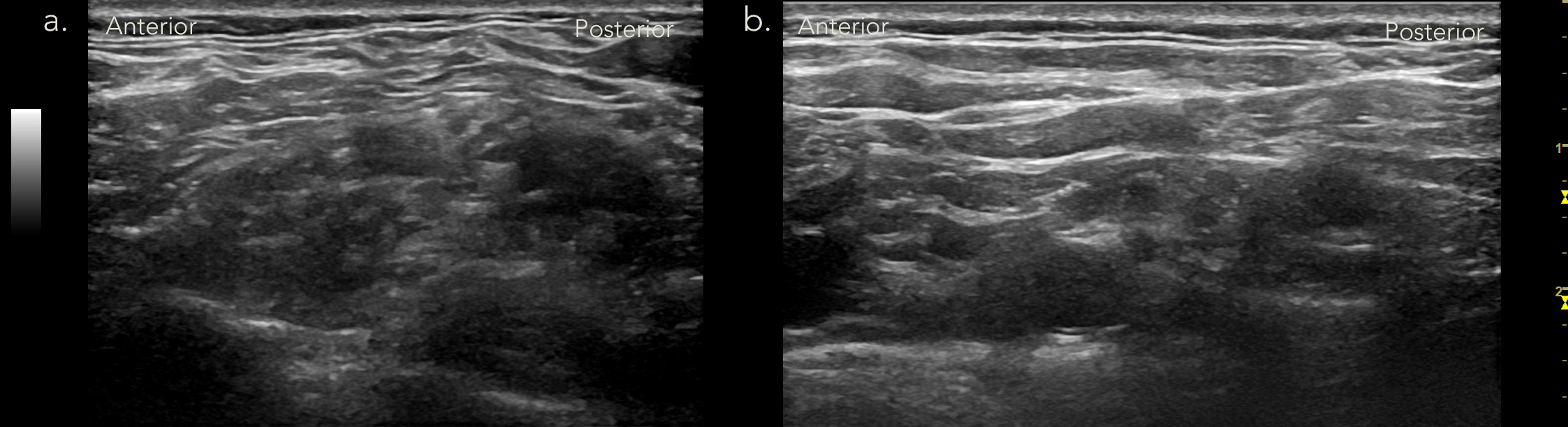
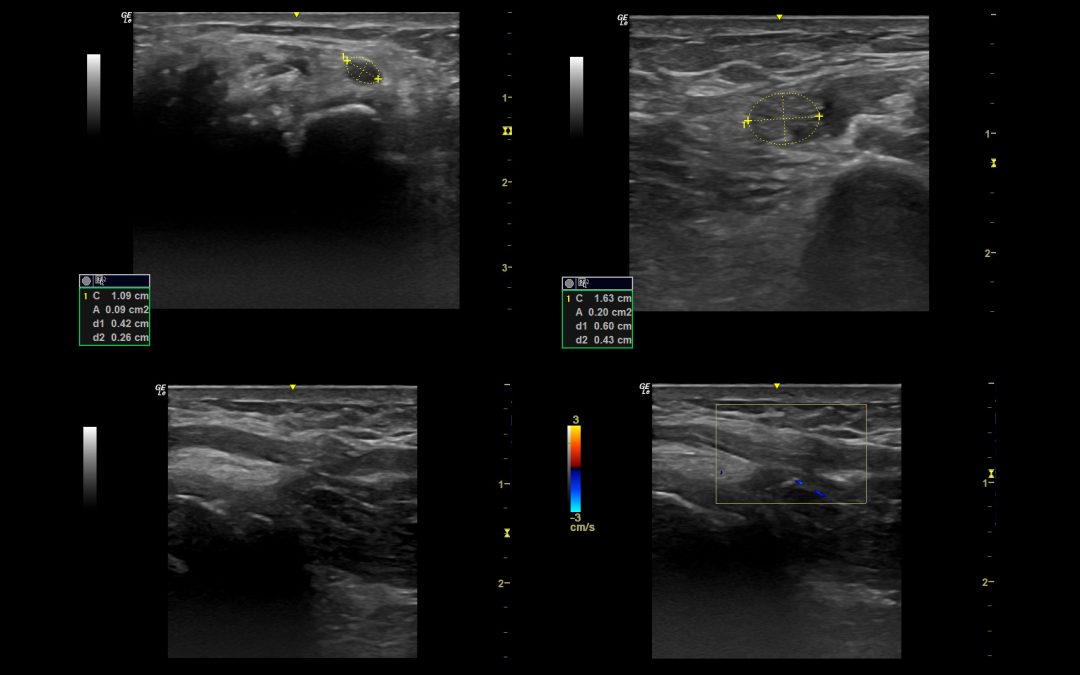
Pic 2. Ultrasound of Guillain-Barre-Syndrome
a. Brachial plexus at interscalene level, showing massive edema, which makes differentiation of roots nearly impossible
b. The same finding in supraclavicular view on the contralateral side.
c. Vasculitic neuropathy
Your first differential in an acute and painful mononeuropathy. Here the symptomatic nerves – often the ulnar or the peroneal – are your choice. Get them along their whole course and either document normal findings at standard sites in still images or the site of lesion including a video. Note that in this case, documentation of possible detectable hypervascularization should also be kept.
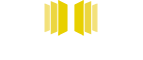
d. Neuralgic amyotrophy
Now it´s getting more tricky. NA often affects the small nerves around the shoulder. You should have a look at the symptomatic nerves – in most cases the long thoracic or the suprascapular nerve. As in the majority of cases NA is unilateral and reference values cannot always be applied for the small nerves, you should opt for side-comparison. Get the symptomatic nerves if this is your suspected diagnosis

Pic 4. Ultrasound in neuralgic amyotrophy
a. enlarged C6 root contribution on affected side (arrow)
b. C6 root contribution on the unaffected side (arrow)

Side note on ultrasound of muscles:
Nerves are interesting, but don´t forget the muscles! They can also help diagnosing nerve damage. Ultrasound is not the most sensitive option for detecting mild neurogenic atrophy, especially in the early stage. But if you have major damage that occurred 2-3 months ago look out for the pattern of neurgenic atrophy!
We hope that was helpful for you. If you have anything to add or comment – we are happy to hear!
See you soon.
Your Sonocampus Team
Want to make sure you never miss a post again?
Sign up for the newsletter

Recent Comments