
This is our very first newsletter for you. We are happy and excited that you take the time to be with us.
In this newsletter we are going to discuss reports published between September and November 2019.
A look into literature reveals one hot topic:
ULTRASOUND OF THE OPTIC NERVE
Before we dive into the latest news, we want to give you a short overview:
Background:
The optic nerve is the second cranial nerve and ontogenetically a part of the central nervous system. It is surrounded by subarachnoidal cerebral fluid and the dura mater (1). This close relation to intracranial conditions makes it a good indicator of intracranial pressure, which is what most studies focus on (for review please see e.g. Tawfik et al. (2), Restrepo et al. 2019 (3), and two very recent reviews: Lochner et al. 2019 (4), Koziarz et al 2019(5)). Reported test characteristics are generally quite good, e.g. Raffiz et al report a sensitivity of 95% and a specificity of 80% in a prospective trial on a neurosurgical ICU, comparing ultrasound to the gold standard of invasive monitoring (6) Furthermore, there are some reports available on optic neuritis, describing a swelling of the optic nerve on the affected eye (for review please see Lochner et al. (7)). Another possible application which was suggested is monitoring of pseudotumor cerebri syndrome (8).
Just to give you an idea of what is going on generally about this topic.
Technique:
Patient positioning: Lying in a supine position with eyes closed
Probe: Linear transducer 7-9 MHz
IMPORTANT: In order not to harm the eye, the power output should be as low as possible with a thermal index of 0.0 and a mechanical index of 0.2 or lower. This can be achieved by reducing power to 30% (2). Many machines already offer a preset for ophthalmologic examination – check out yours.
Probe placement: transverse on the upper eyelid (Figure 1A)
Image obtained:
The optic nerve is visualized as a hypoechogenic tubular structure that appears behind the globe of the eye, surrounded by a hyperechogenic sheath – the optic nerve sheath (Figure 1B)
Measurement:
According to studies carried out in anatomic specimen, the point of maximum swelling of the optic nerve sheath is 3 mm posterior of the globe. At this point, the mean diameter was shown to increase by 60%, while at 10 mm distance it was only 35% (this is why on all ultrasound images of the optic nerve you see two distances marked, as in Figure 1B). Measurement is required to be carried out including the hyperechogenic sheath, as we measure the “optic nerve sheath diameter” (ONSD).
Reference values in literature vary widely, most cut-offs are between 5.0-5.6 mm in diameter.

Figure 1: Probe positioning (1A) and image obtained (1B) in optic nerve ultrasound. Please note measurement of the optic nerve sheath diameter (ONSD) in 1B, which is 3 mm posterior to the globe of the eye
(from: Tawfik E et al. Neuromuscular ultrasound of cranial nerves; J Clin Neurology 2015; 11(2):109*)
But that is enough background information – let´s now look at what happened recently:
OPTIC NERVE ULTRASOUND
TWO RECENT REVIEWS
Koziarz et al. Bedside optic nerve ultrasonography for diagnosing increased intracranial pressure: a systematic review and meta-analysis. Ann Intern Med 2019 Nov 19. Epub ahead of print
CONCLUSION: a normal sheath diameter (ONSD) measurement has a high sensitivity (traumatic brain injury 97%, non-traumatic brain injury 92%) and a low negative likelihood ratio (traumatic brain injury 0.04, non-traumatic brain injury 0.09) that may rule out increased intracranial pressure, whereas elevated measurement, characterized by a high specificity and positive likelihood ratio may be indicated increased intracranial pressure and the need for additional confirmatory tests. The optimal cut-off value for ONSD was 5.0 mm in this meta-analysis.
Lochner et al. Optic nerve sheath diameter: present and future perspectives for neurologists and critical care physicians. Neurol Sci 2019; 40: 2447.
CONCLUSION: ONSD is easy to learn and a safe bedside tool for screening of patients with suspected intracranical hypertension – if increased, they should undergo additional investigations. The review further sums up all other possible indications, e.g. posterior reversible encephalopathy syndrome, bacterial meningitis or encephalitis, acute mountain sickness or optic neuritis. For all of these, further studies are necessary.
PROTOCOL FOR ASSESSMENT OF THE OPTIC NERVE SHEATH DIAMETER
Aspide et al. A proposal for a New Protocol for Sonographic Assessment of the optic nerve sheath diameter: The CLOSED protocol. Neurocrit Care 2019 Oct 3. Epub ahead of print
Aspide et al. address the problem mentioned before: that at the moment we do not have a standardized protocol on HOW to measure the optic nerve sheath diameter. They suggest the “CLOSED protocol” – the abbreviation standing for: Color Doppler-Low power examination – optic disc clarity – short examination duration (safety). They state that their protocol is the result of a narrative review on this topic and the result of expert meetings. The most important news about this review are the definition of recommended settings for US and the use of color doppler for reliable measurement of the ONSD
The most important points about machine settings:
- Frequency of 10 MHz
- Stopping examination if patient reports any discomfort
- Power output 20%-25%
- Depth 40-45 mm (get overview)
- Focus 25-30 mm (site of measurement)
- Gain 55-60% (avoid excessive contrast and less clear images)
- Doppler value of pulse repetition frequency
The color doppler is used to identify the central retinal artery (CRA) and central retinal vein (CRV), which run in the middle of the optic nerve in the distal segment (Figure 2). Further, the ophthalmic artery (OA) is suggested as helpful – which runs parallel to the optic nerve, but outside its sheath. CRA and CRV help identifying the best plane for measurement of the ONSD. The OA helps avoiding overestimation of ONSD by a) identifying an acoustic shadow that fakes a broader hypoechogenic area than there really is and b) a possible tortuous course of the optic nerve – pretending the same.
CONCLUSION: The authors close with the remark that clinical studies are needed to prove feasibility, applicability and sensitivity/specificity of their protocol. But it surely seems a step in the right direction. And if you are just starting out with optic nerve ultrasound, this can surely be a good guideline.
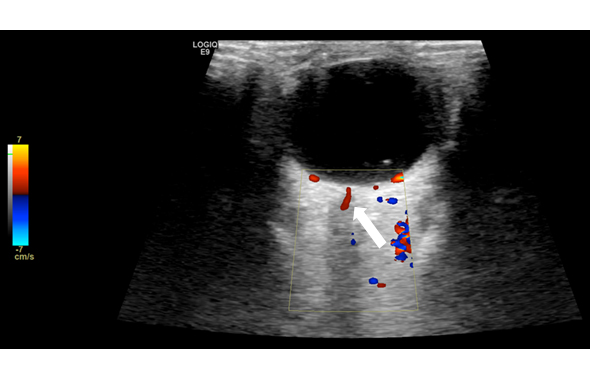
Figure 2: Central retinal artery (white arrow) – suggested as defining the best plane for measurement of the ONSD.
ASYMMETRY OF OPTIC NERVE SHEATH DIAMETER
Naldi et al. Optic nerve sheath diameter asymmetry in healthy subjects and patients with intracranial hypertension. Neurol Sci. 2019 Oct 5. Epub ahead of print
Usually, ONSD values are averaging the measurement of two eyes, but asymmetric ONSD dilation is possible. This would lead to incorrect estimation of intracranial pressure. Lochner et al. therefore looked at how asymmetric the ONSD is in healthy subjects (n=40) compared to patients with intracranial hypertension (20 with idiopathic intracranial hypertension an 20 with intracerebral hemorrhage) on a retrospective basis. Fourty-two of all 80 enrolled subjects showed a significant asymmetry, without significant differences between the groups (p=0.28). The asymmetry was slightly higher in patients than in controls (0.45 mm vs. 0.23 mm, p=0.007). Both, the averaged ONSD as well as the maximum ONSD were higher in patients with IH than in controls (p<0.001). The authors state that interestingly, there was no association between side of the cerebral hemorrhage and the maximal ONSD dilation. They conclude that both – the binocular and the maximum ONSD – may be useful.
CONCLUSION: There is no evidence that measuring and averaging both eyes leads to wrong results.
MULTIPLE SCLEROSIS AND OPTIC NERVE SHEATH DIAMETER
Koraysha NA et al. Evaluating optic nerve diameter as a possible biomarker for disability in patients with multiple sclerosis. Neuropsychiatr Dis Treat 2019 Sept 6; 15: 2571
Koraysha et al. examined OND, ONSD by transorbital sonography and retinal nerve fiber layer and ganglion cell complex thicknesses by optical coherence tomography in patients with relapsing-remitting multiple sclerosis (with history of optic neuritis n=23, without optic neuritis n = 26 and 50 healthy controls). There was no difference between patients and control in OND or ONSD. However, patients with an EDSS score > 2 showed a lower OND and RNFL thicknesses than patients with less disability. They conclude that OND might be a useful biomarker for early disability in RRMS.
CONCLUSION: Further studies needed.
IDIOPATHIC INTRACRANIAL HYPERTENSION
Jeub et al. Sonographic assessment of the optic nerve and the central retinal artery in idiopathic intracranial hypertension. J Clin Neurosci 2019 Sept 17, epub ahead of print
Jeub et al. focused on hemodynamic changes in the central retinal artery before and after lumbar puncture in patients with IIH compared to controls, also taking OND and ONSD into account. They describe an increase of peak systolic velocity and mean velocity in the central retinal artery in IIH patients compared to controls that decreased to normal values after lumbar puncture (only significant for the right eyes). However, there is a wide variability of normal values in literature and also a huge overlap in this study. Therefore, sensitivity and specificity are not overwhelming and so use of theses parameters is not necessary at the moment.
CONCLUSION: see last sentence above.
Enough about the optic nerve – there are other interesting topics:

REFERENCE VALUES FOR CHILDREN AND YOUNG ADULTS
Druzhinin et al. Nerve ultrasound normal values in children and young adults. Muscle Nerve 2019 Sept 14. Epub ahead of print
Druzhinin et al. measured cross-sectional areas of the most common nerves (median, ulnar, radial, cervical roots C5-7, sciatic nerve, common peroneal, tibial, sural) in 72 healthy subjects aged between 2 and 30 years. Age groups were represented as following: 2-4 (n=11), 5-7 (n=15), 8-10 (n=10), 11-13 (n=7), 14-16 (n=7), 17-30 (n=22). They – like two other studies including children before – describe a relatively steady increase of CSA up to the age of 12-14 years (9, 10). Therefore, especially children at these ages should not be assessed with adult reference values. The authors themselves already name the relatively low number of study participants as a major limitation.
CONCLUSION: Small number of participants surely a problem, but their study confirms previous findings and therefore seems a good point to start from when assessing children.
NEURALGIC AMYOTROPHY & HEPATITIS E
Arányi et al. Multiphasic presentation of neuralgic amyotrophy associated with hepatitis E virus infection. Muscle Nerve 2019 Oct 1. Epub ahead of print.
Just to draw your attention to it: A case series (n=3) of Aranyi et al. highlighting that a) a multiphasic presentation and b) multiple nerve involvement in patients with neuralgic amyotrophy seems to be a hint towards concomitant infection with the hepatits E virus.
CONCLUSION: There are more studies on that topic. Just think about Hepatitis E when encountering a patient with an atypical course of neuralgic amyotrophy!
Ok, that was a very focused summary 🙂 We hope you can use it. If you think we missed an important point or you have further questions, please leave a comment.
Your Sonocampus Team
References:
- Helmke and Hansen. Fundamentals of transorbital sonographic evaluation of optic nerve sheath expansion under intracranial hypertension. Pediatr Radiol 1996; 26(10): 701
- Tawfik E., Walker F., Cartwright M. Neuromuscular ultrasound of cranial nerves. J Clin Neurol 2015; 11 (2): 109
- Restrepo J, León OJ, Quevedo Florez LA. Ocular Ultrasonography: a useful instrument in patients with trauma brain injury in emergency service. Emerg Med Int 2019: 9215853*
- Lochner P, Czosnyka M, Naldi A, Lyros E, Pelosi P et al. Optic nerve sheath diameter: present and future perspectives for neurologist and critical care physicians. Neurol Sci; epub ahead of print (published online: July 31st, 2019)
- Koziarz et al. Bedside optic nerve ultrasonography for diagnosing increased intracranial pressure: a systematic review and meta-analysis
- Raffiz M and Abdullah JM. Optic nerve sheath diameter measurement: a means of detecting raised ICP in adult traumatic and non-traumatic neurosurgical patients. Am J Emerg Med 2017; 35 (1): 150
- Lochner P, Leone MA, Coppo L, Nardone R, Zedde ML, Cantello R, Brigo F. B-mode transorbital ultrasonography for the diagnosis of acute optic neuritis. A systematic review. Clin Neurophysiol 2016, 127 (1): 803
- Lochner P, Fassbender K, Lesmeister M, Nardone R, Orioli A, Brigo F, Stolz E. Ocular ultrasound for monitoring pseudotumor cerebri syndrome. Journal of Neurology 2018; 265: 356
- Cartwright MS, Passmore LV, Yoon JS, Brown ME, Caress JB, Walker FO. Cross-sectional area reference values for nerve ultrasonography. Muscle Nerve 2008; 37: 566
- Zaidman C, Al Lozi M, Pestronk A. Peripheral nerve size in normal and patients with polyneuropathy: an ultrasound study. Muscle Nerve 2009: 40: 960
*This is a free article!

What's up, always i used to check weblog posts here early in the daylight, for the reason that i enjoy to learn more and more.| а
Maybe you want to check out the new case?