
Dear readers,
Welcome to our second newsletter. Spring is just starting out here, usually the most beautiful time of the year, but now we are all trapped in those crazy times, with a virus holding us all hostage all over the planet.
We would like to start with a “Thank you” to all of you, who are keeping medical systems up and running throughout the planet. And we all hope that our lives can soon return to normal.
Meanwhile we will provide you with our overview – let´s talk about the most recent publications in the field of neuromuscular ultrasound.
A look into literature shows a quite diversified picture, which cannot be summarized under one common topic. Altogether there were no big or life-changing studies published in the past three months, but some interesting reports about ongoing work that we would like to direct your attention to.
As always please note that we can just pick out a few papers. If we missed your most important paper from the past months – just let us know.

REFERENCE VALUES FOR CHILDREN
We are proceeding with reference values for children (please also see our Newsletter Winter 2019):
*Sonographic measurements of normal C5-C8 roots in children
Wang W. and Wang Q. Muscle Nerve 2020, epub ahead of print
This is a big study with open access in 441 children from newborn to the age of 18, also describing the special points when scanning small children.
Conclusion:biggest cohort available – good start if you are in the topic and don´t have your own reference values ready.
Nerve ultrasound reference data in children from two to seven years
Schubert et al. Clin Neurophysiol 2020. Epub ahead of print.
Another study, examining 116 children, this time younger (from 2 to 7 years old) and looking at many nerves: median, ulnar, tibial, fibular, sural, radial, vagus, C5 and C6.
They also describe the 30% side variation in CSA in healthy children – a finding that also accounts for adults.
POLYNEUROPATHIES
Nerve ultrasound imporves detection of treatment-responsive chronic inflammatory neuropathies
Herraets et al. Neurology 2020. Epub ahead of print
This study examined 100 consecutive patients with suspected chronic inflammatory neuropathy. The diagnosis was reached by
a) Fulfillment of clinical criteria for CIDP/MMN of the EFNS/PNS AND
b) A clinical course fitting CIDP/MMN during a 1 year follow-up AND
Either:
c) NCS abnormalities in accordance with EFNS/PNS criteria OR
d) Nerve ultrasound abnormalities with treatment response.
In 38 out of 100, the diagnosis of a chronic inflammatory neuropathy could be established. In addition, 15 patients with NCS not meeting the criteria but showing abnormalities in ultrasound were treated – of which 8 had a treatment response. The authors therefore argue that ultrasound is a good additional tool that could shorten the time to diagnosis and treatment. The added value of US was 21%.
Further, they found a very high sensitivity for US and a very high specificity for NCS – which makes them complementary tools that should be used together in clinical suspicion of CIN.
Neuromuscular ultrasound for taxane peripheral neuropathy in breast cancer.
Lycan et al. Muscle Nerve 2020. Epub ahead of print
A study on 20 patients with self-reported symptoms with taxane chemotherapy-induced peripheral neuropathy, compared to historical controls. The main finding was a reduction in CSA of the sural nerve that also correlated with intraepidermal nerve fiber density. The other scanned nerves (tibial and median) did not exhibit any significant difference between patients and controls.
Conclusion:No direct influence on your daily work. But reduction of CSA is an uncommon finding, that was up to date described in spinocerebellar ataxia syndrome – which, like taxane, cause a neuronopathy and not the distal dying back of e.g. metabolic polyneuropathies. Maybe we are also moving forward in this direction.
*Very early Guillain-Barré-Syndrome: a clinical-electrophysiological and ultrasonographic study
Berciano et al. Clin Neurophysiol Pract 2019; 5: 1-9
A retrospective case series that investigated 15 patients with GBS in the very early phase – at least the electrophysiologic examination, which was carried out the first time at a maximum of four days after symptom onset. Ultrasound was carried out within the first two weeks after disease onset. Reports on GBS are quite rare, which is why we would like to bring this to your attention.
The important things to keep in mind:
- 12 out of 14 patients who underwent ultrasound had abnormalities at cervical root level
- The pathological finding was a variable combination of symmetric or asymmetric blurred boundaries and significant increase in CSA.
So in GBS do not only look for swelling, but also for loss of the physiologic hyperechogenic rim!
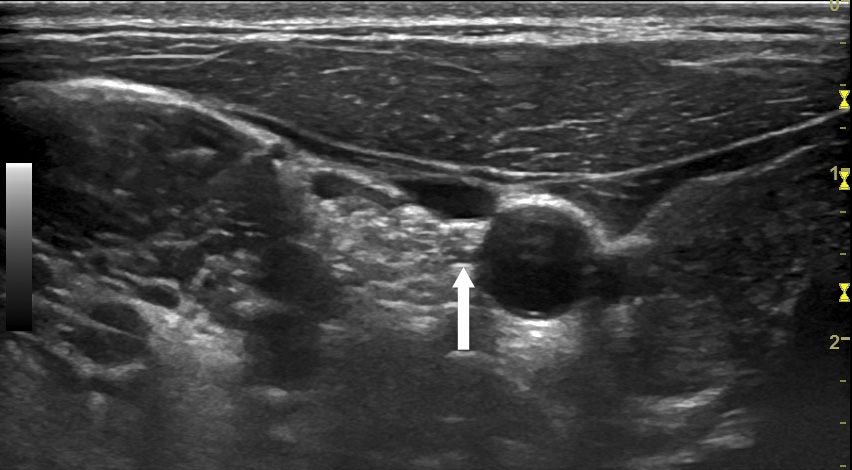
Please find an example of an own patient below:
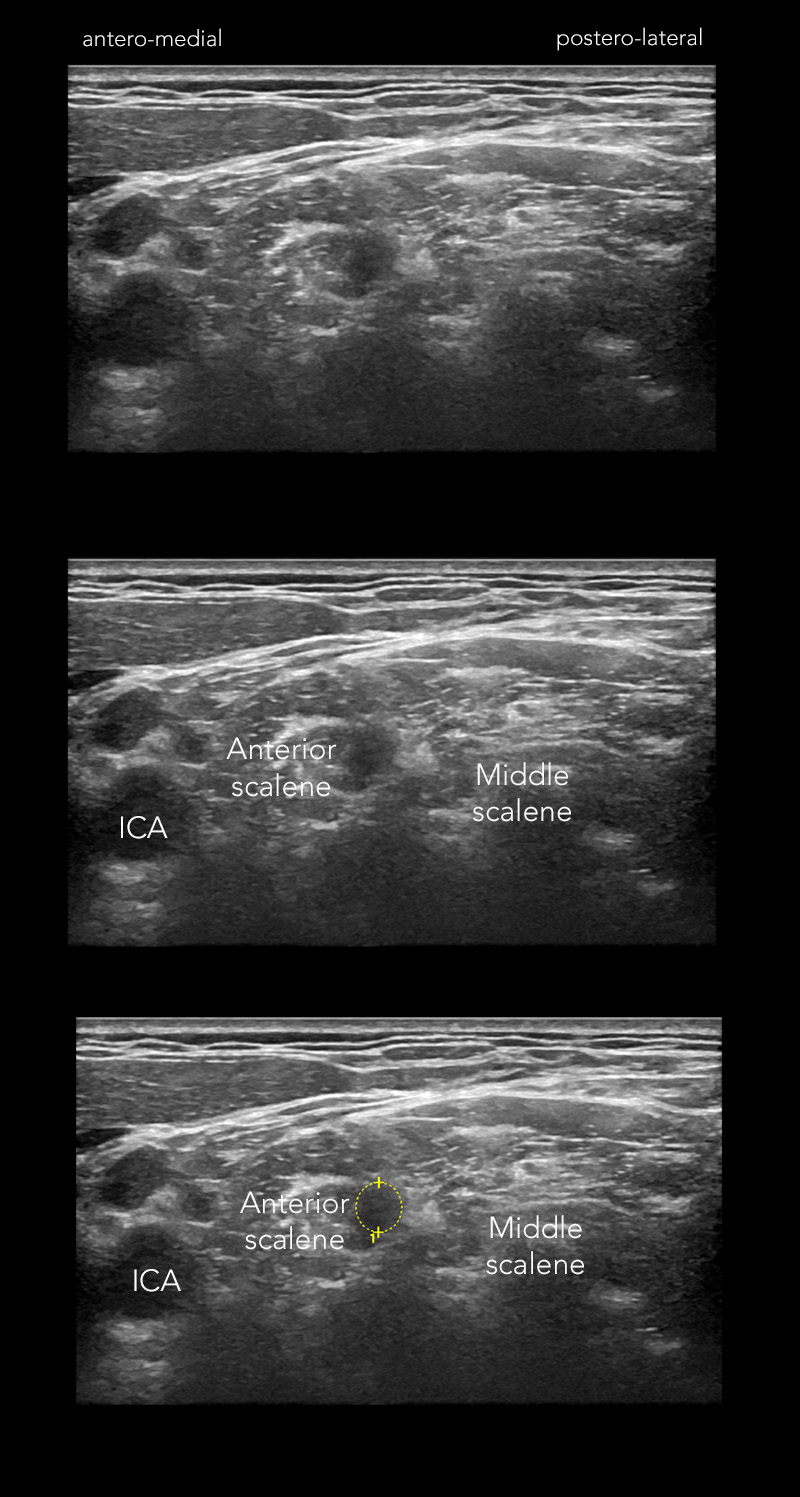
Figure 1: Transverse view of the left C6 root in a 27 year old male with GBS, two days after symptom onset. Nerve conduction studies were still normal at this point. Note the blurred border of the root, which makes it hard to differentiate from the surrounding muscle – much harder, that you would expect in a young, slender male.
NERVE TRAUMA
Neuromas and postamputation pain.
Buch et al. Pain 2020. Epub ahead of print.
The study looked at 67 amputees. Neuromas were found with ultrasound in 53% of them. 47 of 57 (82%) had pain and 6 of 10 (60%) did not. The authors concluded that it is not the presence of neuromas that drives postamputation pain.
SMALL NERVES
*Transient postsurgical gastroparesis is accompanied by reversible changes of the cervical vagus nerve´s morphology after neck dissection – an ultrasound study
Özcaglayan and Ersözlü. Med Ultrason 2020; 22 (1): 26-30
The authors prospectively investigated a cohort of patients undergoing neck dissection, correlating diameter/CSA of the vagus nerve preoperatively, one week and one month after neck dissection to symptoms of postsurgical gastroparesis.
They found a transient increase in diameter and CSA one week after surgery, that remitted to preoperative levels after one month and correlated with gastrointestinal symptoms.
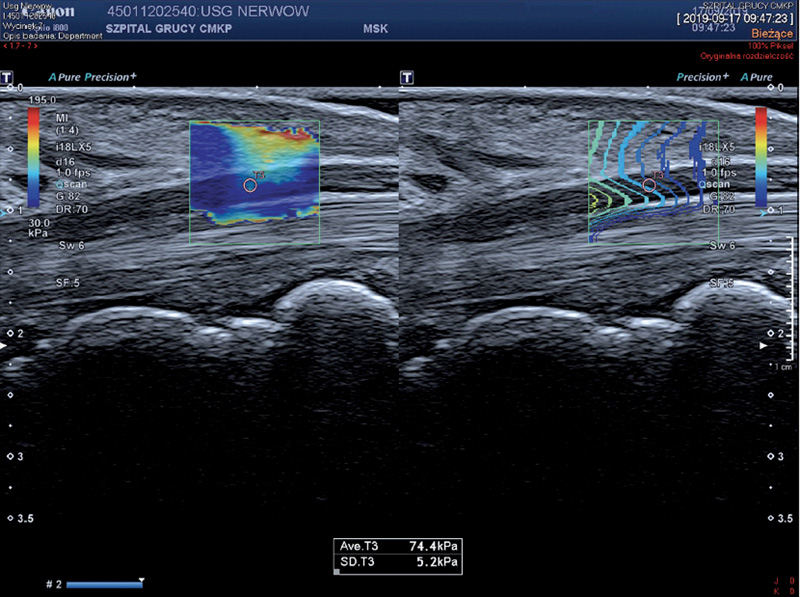
From: Zakrzewski et al, Pol J Radiol 2019; 84; e581-591
ELASTOGRAPHY
Influence of limb position on assessment of nerve mechanical properties using shear wave elastography
Rugel et al. Muscle Nerve 2020
Elastography is an emerging technique in assessment of peripheral nerve impairment working with alteration of mechanical tissue properties as surrogate marker. Shear wave elastography assesses the speed at which shear waves travel through tissue – but not only changes in nerve architecture influence the result. Plane of measurement and tension may also contribute.
Therefore this study assessed SW velocity in the median and ulnar nerves at proximal and distal sites of sixteen young, healthy adults in two positions: elbow flexed 90° and extended 180° – the former exerting more tension on the ulnar, the latter on the median nerve.
The important thing is: there was an increase of SW velocity in the ulnar nerve of 91% at proximal and 89% at distal site in the flexed position. The according numbers for the median nerve were 89% and 64% in extended position.
Conclusion:elastography is progressing – but we need to learn a lot more about standardization before using this technique routinely.
*Ultrasound elastography in the evaluation of peripheral neuropathies: a systematic review of the literature
Zakrzewski et al. Pol J Radiol 2019: 84: e581-91
A free article in which you can get an overview which studies are published on the topic of elastography of peripheral nerves and for which disorders the technique is currently under evaluation. The conclusion is the same as in all articles on this topic: we are far from being able to use elastography of peripheral nerves in our daily diagnostic routine. But we are on our way to find out.
We hope that was informative for you. Feedback is welcome as always.
We wish you the best during these hard times. Stay safe.
Your Sonocampus Team
*This is a free article
Recent Comments